For Mindlovesmisery’s Saturday Mix: double take.
he’s lain in the lane
on the hill, he’s a heel
waking drunk, he’ll wonder
has he the will to heal?

For Mindlovesmisery’s Saturday Mix: double take.
he’s lain in the lane
on the hill, he’s a heel
waking drunk, he’ll wonder
has he the will to heal?

Centrum Voiceworks last week. I did not get a wonderful photograph of the Reverend Robert B. Jones, Sr. He was moving and I did not want to use a flash! He did two classes a day, an am blues class and an afternoon gospel class. They wove together. He talked about how the pentatonic scale came with enslaved Africans and met the European music and produced spirituals, praise songs, the blues and gospel. He also spoke about how the early blues musicians were playing acoustic guitar in noisy places, so the guitar was rhythm, harmony and bass, all at once. He traced how the changes in circumstances is reflected in the changes in music in the United States and how musicians of all races and creeds influence each other. He talks about the history of music as healing.
I didn’t get a great photograph of him, but here is another student:

And here is the teacher, engaged:

Thank you, Reverend, for your amazing classes, singing, guitar playing and the final blues jam after the concert on Friday night!

A patient of mine saw a cardiologist recently.
His previous cardiologist has retired. The patient had a cardiac bypass in the past, he has a stent, he has known coronary heart disease and he’s in the young half of my practice. That is, under 60.
He had not seen a cardiologist for 2-3 years because he had a work injury, worked with Labor and Industries, the case was closed, he couldn’t go back to work, he found a lawyer. He lost his regular health insurance along with the job, so couldn’t see the cardiologist.
The L & I case is reopened. A physiatrist recommended specific treatment that was not done, and that allowed the case to reopen.
The specific treatment center then notes that he has heart disease and that he needs clearance from a cardiologist. I set him up with a new cardiologist.
“How was the visit?” I ask.
He shrugs. “The staff was nice.”
“I have the note.”
“The cardiologist spent under ten minutes with me. It was clear that she was rushed. She did not seem very interested. It was difficult to get my questions answered.”
“Her note is six pages.”
He snorts. “Great that she could get a six page note out of that visit.”
“Do you want a copy?”
“No.”
He is cleared for the specific treatment.
I have no doubt that the cardiologist spent more than 6-8 minutes on his visit and his note. But not in the room. Other people are entering the information filled out in the waiting room, medicines, allergies, past medical history, family history. Hopefully the cardiologist is reading my note and letter. But the problem is, doctors aren’t doing it in the room. So the impression left with the patient is that we spend 6-8 minutes on their visit, we are late, we are rushed. Doctors are looking at data. They are not listening to patients.
Medical Economics, a journal that arrives without me asking for it, says over and over that we need more physician “extenders”, that we need to have people doing the data entry, people doing the patient teaching, more people and machines….No. They are wrong. We need LESS barriers between us and the patients, not MORE. We need more time with patients. Every single extender we add burns physicians out more, because the salary has to be paid AND more patients seen faster to do that AND we are still ultimately responsible for knowing and reading and absorbing every single piece of information that is placed in that patient’s chart. An extender is NOT an extension of my brain and an extender is another person I have to communicate with and train.
Just. Say. No. to the managers who pile MORE barriers between the physician and the patient. NO.
It just makes me so mad that he lost his health insurance BECAUSE he got injured at work and so then his heart disease goes untreated as well… can’t afford medicines…if he then has a heart attack while uninsured we lifeflight him to Seattle, it costs a fortune, he loses his house and property and then is on medicaid and may end up on permanent disability, and what are the chances he returns to work? The US medical corporate money grubbing is insane. Single payer, medicare for all, make the US great again.

For photrablogger’s Mundane Monday #148: clothes hanging.
I was out from work very sick in 2012. I had strep A in lungs and muscles, including throat muscles. I could not talk. I put my hammock up in a tree, high up. There was no one to talk to there, just the leaves and wind and birds and sky.
And here are some socks and another view:

I could watch the deer from the tree.

It was a very good place to be quiet and heal.


“Please write something from a medical perspective about anxious people who worry every little thing is some serious disease.” — reQuest 2018
This is quite a brilliant and timely question.
Here: https://www.anxiety.org/hypochondriasis-replaced-by-two-new-disorders-in-dsm-5.
The DSM V was published on May 18, 2013. This is the Diagnostic and Statistical Manual of Mental Disorders version 5, and it redefines various disorders. For example, opiate dependence has disappeared and so has opiate addiction. Instead, there is one diagnosis: opiate overuse syndrome. Which really combines both opiate addiction and opiate dependence and makes it a spectrum.
The DSM V drops hypochondriasis. Wait, you say, that diagnosis no longer exists? Well, yes, correct. So the diagnoses are made up? Yes, as my daughter says, “All the words are made up.” So psychiatry changes and the diagnosis definitions change and some diagnoses disappear. Medicine is like the Oregon Dunes, really. The information is changing daily. I went into medicine thinking it is like a cookbook, where I just have to learn all the recipes. Nope, sand dunes: the wind and waves and new information change the contours daily. It drives my patients nuts. “My insurance won’t cover the medicine I’ve been on for 26 years.” Um, yeah, sorry, work for single payer and shut down the insurance companies, ok? “This combination of medicines has never killed me yet.” Um, yeah, sorry, but you are in fact getting older and we no longer think that combination is safe and first do no harm: I can’t prescribe combinations that I think may kill you.
Hypochondriasis has been replaced by two diagnoses: Somatic Symptom Disorder and Illness Anxiety Disorder.
From the Mayo Clinic website: https://www.mayoclinic.org/medical-professionals/clinical-updates/psychiatry-psychology/diagnostic-statistical-manual-mental-disorders-redefines-hypochondriasis.
“Patients with illness anxiety disorder may or may not have a medical condition but have heightened bodily sensations, are intensely anxious about the possibility of an undiagnosed illness, or devote excessive time and energy to health concerns, often obsessively researching them. Like people with somatic symptom disorder, they are not easily reassured. Illness anxiety disorder can cause considerable distress and life disruption, even at moderate levels.”
“To meet the criteria for somatic symptom disorder, patients must have one or more chronic somatic symptoms about which they are excessively concerned, preoccupied or fearful. These fears and behaviors cause significant distress and dysfunction, and although patients may make frequent use of health care services, they are rarely reassured and often feel their medical care has been inadequate.”
So, subtle difference. Broadly, the illness anxiety disorder people are sure they have SOMETHING and are worried about ALL THE SYMPTOMS. The somatic symptom disorder people are worried about A SPECIFIC SYMPTOM OR SYMPTOMS and WHY HAVEN’T YOU FIXED ME.
Some of the people complaining of weird symptoms do have a medical diagnosis that has not been sorted out. Take multiple sclerosis for example. The average time from the start of symptoms to diagnosis is 4-5 years.
Here: http://biketxh.nationalmssociety.org/site/DocServer/Facts-about-MS.pdf?docID=54383).
Also here: https://www.nationalmssociety.org/Symptoms-Diagnosis/Diagnosing-Tools.
Another one is sarcoidosis: https://www.mayoclinic.org/diseases-conditions/sarcoidosis/symptoms-causes/syc-20350358. It’s hard to diagnose, can affect different parts of the body, and it’s still pretty mysterious. Add to that list chronic fatigue, fibromyalgia, chronic pain, and numerous other diagnoses.
With multiple sclerosis, you may be thinking, well, if they had just done the brain MRI sooner, the diagnosis would be made. Not necessarily. I did find a patient with a bunch of MS brain lesions: made the diagnosis. She had had a brain MRI 3-5 years before because of suspicious symptoms during pregnancy. At that time her MRI was entirely normal.
The DSM V does not have a diagnosis called psychophysiological disorder. This is an ongoing discussion:
1. https://pdfs.semanticscholar.org/7f7f/21a9b524fb677d575428bea11aab4c8d70c5.pdf
2. https://thoughtbroadcast.com/2011/01/21/psychosomatic-illness-and-the-dsm-5/
This site: http://www.stressillness.com/ is my current favorite about psychophysiological disorders. I heard a lecture from the physician who runs the site. He is at OHSU in Portland and gets the gastrointestinal patients where “they can’t find anything wrong” from all over the state. He is really good at this. He and I are in agreement: the symptoms are real. However, the symptoms may come from emotional suffering and from emotional trauma in the past and present.
It is clear that fibromyalgia is a “real” disorder: functional MRI of the brain shows the pain centers lighting up more with a standardized pain stimulus than “normal” patients. PTSD is “real”. It is interesting that there is more stigma surrounding fibromyalgia and chronic fatigue than PTSD: is that because the former two are more often diagnosed in women, and the latter is legitimate (finally) for male (and a smaller number of female) veterans?
And what do I, your humble country doctor, think? I think that chronic fatigue and PTSD and fibromyalgia and illness anxiety disorder and the others all may be variations of the same thing. Our body will handle and “store” or “stuff” emotions that we cannot handle or are not in a safe situation to handle it. Eventually our body decides that we are now safe enough and will notify us that we have to handle the emotions. Currently our culture is terribly unsupportive of this and there is huge stigma attached to dealing with it. We are all supposed to just be nice.
In the end, we can’t judge how a friend feels or whether they are well or not. We have to treat them with respect and kindness.
The photograph is me on my grandfather’s lap. He became a psychiatrist and I am a family physician. Taken in 1962 or 3. We are at cabins in Ontario, Canada. What a pair of grubs, but happy…..

…on me…
For Wordless Wednesday.
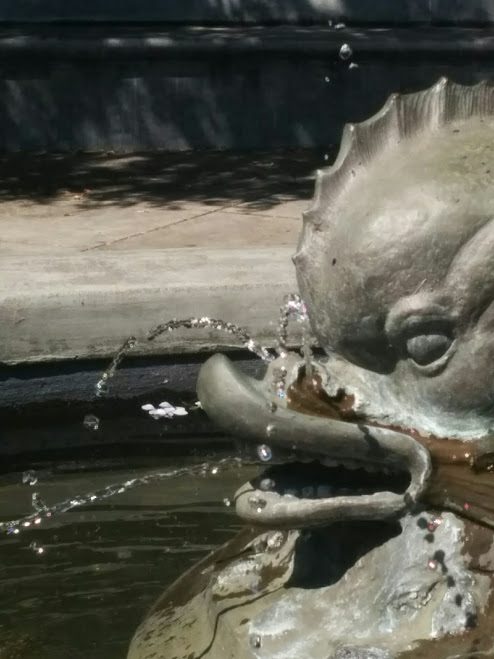
This is our Galatea Fountain again: the fountain is cooling and the sound of the water is delicious on a hot day. I hope it cools the eclipse hunters, but even more, I hope hatred and discrimination and anger and bigotry cool and slide away in healing and love.
Two steps forward and one step back: I hope we lurch towards peace.

When we left about 45 minutes later, the song sparrow was not on the sidewalk any more. It was in this tree. I didn’t see it at first, I heard it. It was still acting a little stunned, because it was trying to sing and was only managing the first three notes of it’s song. Hopefully it will fully heal!

Two days ago we came across this song sparrow on the sidewalk below a windowed walkway. Stunned, we thought. Not dead. I poured a little water on the sidewalk just in front of the bird and left it alone. It moved its’ head a tiny bit.
Part two here: https://drkottaway.com/2017/07/14/flown/
BLIND WILDERNESS
in front of the garden gate - JezzieG
Discover and re-discover Mexico’s cuisine, culture and history through the recipes, backyard stories and other interesting findings of an expatriate in Canada
Or not, depending on my mood
All those moments will be lost in time, like tears in rain!
An onion has many layers. So have I!
Exploring the great outdoors one step at a time
Some of the creative paths that escaped from my brain!
Books, reading and more ... with an Australian focus ... written on Ngunnawal Country
Engaging in some lyrical athletics whilst painting pictures with words and pounding the pavement. I run; blog; write poetry; chase after my kids & drink coffee.
Coast-to-coast US bike tour
Generative AI
Climbing, Outdoors, Life!
imperfect pictures
Refugees welcome - Flüchtlinge willkommen I am teaching German to refugees. Ich unterrichte geflüchtete Menschen in der deutschen Sprache. I am writing this blog in English and German because my friends speak English and German. Ich schreibe auf Deutsch und Englisch, weil meine Freunde Deutsch und Englisch sprechen.
En fotoblogg
Books by author Diana Coombes
NEW FLOWERY JOURNEYS
in search of a better us
Personal Blog
Raku pottery, vases, and gifts
𝖠𝗇𝗈𝗍𝗁𝖾𝗋 𝖶𝗈𝗋𝖽𝖯𝗋𝖾𝗌𝗌.𝖼𝗈𝗆 𝗌𝗂𝗍𝖾.
Taking the camera for a walk!!!
From the Existential to the Mundane - From Poetry to Prose
1 Man and His Bloody Dog
Homepage Engaging the World, Hearing the World and speaking for the World.
Anne M Bray's art blog, and then some.
My Personal Rants, Ravings, & Ruminations
You must be logged in to post a comment.