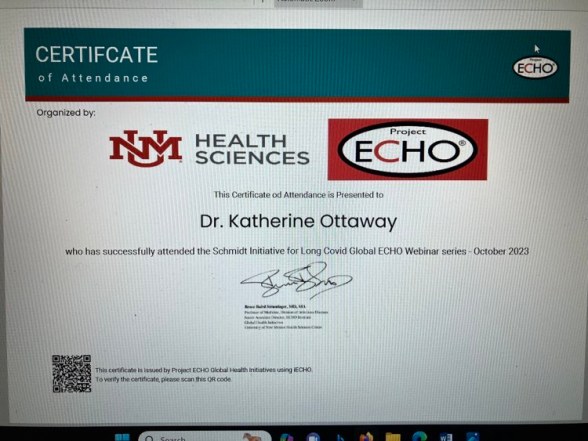
The latest Schmidt Initiative iECHO Long Covid zoom two days ago is by Hannah E. Davis, MPS, the co-founder of the Patient Led Research Collaborative (PLRC).
She got Covid-19 in March of 2020. Her first sign that something was really off was that she couldn’t read a text message. She thought that most people recover in two weeks so didn’t do much about it. She went on to clotting and neurocognitive problems and MECFS.
Her job and expertise were in machine learning data sets. As she realized that she was really sick and was not improving, she also realized that Long Covid was not even on the radar for physicians, overwhelmed by the acutely ill and dying. She started the interdisciplinary team co-led by four women and with over fifty patient researchers. The group is 61% women and 70% disabled.
They published an op ed piece about the body politic in the New York Times in April of 2020. By May of 2020 they had a fifty page article out documenting that even mild cases of Covid-19 could cause long term impacts. They describe multiple symptoms long term, not just respiratory. They also noted and documented medical stigma happening and were instrumental in changing the dialog from anecdotes of non-recover to data about non-recovery.
In June to August of 2020 they appealed the the World Health Organization (WHO) with a video message presenting data about long term effects.
In December of 2020 they presented a paper characterizing Long Covid. There are now 3-4 biomedical papers coming out each day.
She states that there are multiple myths about Long Covid: “It’s mysterious, we don’t know anything about it.” is not true. She listed other myths, but I have to go back through the slides.
The group is still highly active in research and is advocating for patient involvement in research. They have developed score cards for the level and quality of patient engagement. Tokenizing gives a score of -1 or -2, where instead of patient engagement in all stages of the research project, they are told “Come look at our final paper and give us the patient engagement gold star.” That is not adequate engagement. Other diseases have also made patients push for engagement in research: HIV, Parkinsons, PANDAS and more. Patients just want to get better and they want research that matters.
Worrisome data include that 10-12% of vaccinated people who get Covid-19 still can get Long Covid. This is less than the unvaccinated, but it’s still one in ten.
Their data shows that the majority of that 10-12% are not recovered at one year.
Another myth is that there is no treatment, but there are treatments at least for symptom management.
They published the Long Covid paper in the January 2023 Nature, documenting the many many symptoms and ongoing early stage treatments, many taken from other diseases such as MECFS.
One third of people who get Long Covid do NOT have preexisting conditions. It attacks all ages, women more then men, and prior infection may increase risk. Respiratory problems are more likely to recover, barring lung scarring. 43% of Long Covid patients report a delayed onset of neurocognitive symptoms.
Regarding mental health, research shows that stigmatization is still common and that patients who have experienced that are more likely to be depressed, anxious or even suicidal. In contrast, even one non-stigmatizing encounter, medical or family or friends, makes people have lower rates of depression, anxiety or suicidal ideation.
It is abundantly clear that this is a biomedical illness. Enabling google research will allow those papers to be delivered daily. I am on a list where I get daily reports of Covid-19 research and papers.
Next she talked about the current treatments, many taken from other similar illnesses. I have to say that the microclots scare me the most. There are clinical trials ongoing as well as amazing bench science, but meanwhile physicians need to listen to patients, believe them, pay attention to the ongoing research and help patients.
I spoke to a provider yesterday that I last saw two years ago. I said I wanted to work with Long Covid patients. “Good!” he said, “Because I don’t want to!” I think that attitude may be very wide spread.
I also looked at our county (and only) hospital’s page on Covid-19. There is not ONE WORD about Long Covid. Isn’t that interesting? Denial ain’t just a river in Egypt.
This is just what I got from the lecture. There was and is more. Physicians and patients can attend and they file the talks so that you too can watch them. Here:
https://hsc.unm.edu/echo/partner-portal/echos-initiatives/long-covid-global-echo.html
Blessings.